HAVE YOU EVER had PAIN ON YOUR HEEL AFTER RUNNING? EVER NOTICED PAIN DURING RUNNING? STARTED RUNNING MORE FREQUENTLY?
Continuing from our running series and its related injuries, today we explore another common site of injury, the heel and base of foot. As mentioned previously, running is one of the most common source of exercise people go to when it comes to fitness. Runners would often spend countless hours hammering their feet onto hard surfaces in order to reach their goals, whether that be strengthening, stamina or cardiovascular fitness.
As explored in our previous posts, running injuries have become quite a common theme in our clinics recently due to the current COVID-19 situation. As a result of this, heel pain has been increasing amongst our patients. The most common source of heel pain is often referred to as plantar fasciitis/plantar heel pain and below we explore what that is, how it occurs and what can be done for it.
WHAT IS PLANTAR FASCIITIS (PF)/PLANTAR HEEL PAIN?
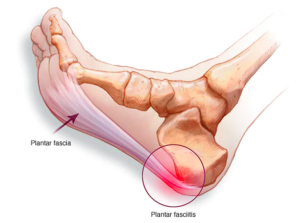
Plantar fasciitis is often a term used for the inflammation of the plantar fascia ligament on the base of the foot. In the term plantar fasciitis, it can be broken down into 3 sections, ‘plantar’ meaning bottom of feet, ‘fasci(a)’ meaning the band of tissue/ligament at the base of foot and ‘itis’ meaning inflammation. Plantar fasciitis is commonly characterised by pain along the plantar surface of the foot which is often worse when walking or running.
Along the bottom of our foot runs a long thick band of tissue/ligament that connects the heel to the base of the foot. It’s primary function is to provide flexibility and stability for the foot, often referred to as the “windlass effect”.
Commonly, plantar fasciitis has been associated with the inflammation of these ligaments, hence the term fasciitis, however recently studies have shown that inflammation may or may not be present with this condition. Instead, it has shown that there may be some degree of wear and tear of these tissues at the bottom of the foot in conjunction with or without inflammation. As a result of this, plantar fasciitis (PF) is commonly associated with the term plantar heel pain and it’s management has incorporated different concepts such as strengthening into the mix.
Why do we get Plantar fasciitis?
The cause of the PF or plantar heel pain is poorly understood due to its vast array of plausible causes. The most common concept behind the development of PF is derived from overuse injury to this band of ligament causing repetitive straining or micro-tearing.
Common causes of PF include:
- Excessive running/walking
- Recent increase in distance and frequency of running/walking
- Faulty running shoes
- Flat feet (pes planus) or High arching feet (pes cavus)
- Poor ankle mobility due to tight calf muscles
- Prolonged standing on hard surfaces
- Increased BMI/weight
CHARACTERISTICS/SYMPTOMS OF PLANTAR FASCIITIS:
- Heel pain or pain along inside of heel
- Tenderness in the morning or within first step
- Limited ankle dorsiflexion due to tight calves
- Noticeable limp when walking
- Pain worse when walking on hard surfaces or footwear
- Pain worse when running/walking
- Relieved via rest/non weight-bearing
What can you do about PF/Plantar heel pain?
PF can be quite a debilitating condition if left untreated or treated improperly. 90% of patients who suffer from PF would often notice drastic improvements to their condition/symptoms within 10 months of starting simple treatment methods/physical therapy.
1. Initial therapy – REST, ICE, NSAIDs
As PF is an overuse injury that has often developed due to repetitive stress to the ligament, we should listen to our body when it’s hurting, know why it’s hurting and how to reduce that overuse. With PF, it’s important that we find adequate rest from aggravating activity. Decreasing or ceasing any running/walking or aggravating activities that force the feet to slam onto hard surfaces is a good start.
Secondly, using an ice bottle to roll over the base of the foot has been shown to be very effective in helping reduce the pain caused by PF.

Lastly, taking NSAIDs or anti-inflammatories can help with the reduction of pain and inflammation if present. Medication should always be taken with caution and should you have any concerns, please don’t hesitate to consult with your doctor.
2. Stretching and self-massage
As PF develops, one of factors involved in this development is tight calves. Stretching out the calves and lower leg and foot muscles is a simple and effective way to help relieve some tension through the foot and ankle, ultimately providing some relief.


Additionally, if you have some moisturising cream at home or any mild lubricant, you may apply some self-massage along the base of the foot, along the plantar fascia and across some of the foot muscles at the base. Always be mindful of the irritation that may occur when doing this and should never be more than a 3/10 pain rating.

3. Strength
As we see improvements to pain related to PF, it is crucial that we continue to build up strength in our lower leg and foot to help support and improve the biomechanics of our feet. Working on big toe and calf muscle coordination and strength has shown to aid in reduction of pain and improvement in function.


4. Get assessed and managed
As PF can be quite debilitating if left untreated, studies has shown that physical therapy can aid with recovery and give good results. There is a lot of causes that can attribute to the development of PF and it’s very beneficial to have it looked at earlier rather than later. Understanding why PF occurs, what are the main causes of it and how to properly manage it is the key to success. Here at Health House Clinics, we treat each individual differently and cater all our management program based on each individual. As PF can be attributed to different causes, it is pivotal to have it looked at and get a tailored treatment regime to help aid in recovery.
If you would like to find out more, please don’t hesitate to contact us on (02) 9524 8862 or email us at info@healthhouseclinics.com.au.
References:
Buchbinder. B (2021), Plantar Fasciitis, Isaac. Z, Curtis. M (Ed.), UpToDate. Retrieved September 16th 2021, from https://www-uptodate-com.simsrad.net.ocs.mq.edu.au/contents/plantar-fasciitis?search=plantar%20fasciitis&source=search_result&selectedTitle=1~40&usage_type=default&display_rank=1
Lemont H, Ammirati KM, Usen N. Plantar fasciitis: a degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc 2003; 93:234.
Jarde O, Diebold P, Havet E, et al. Degenerative lesions of the plantar fascia: surgical treatment by fasciectomy and excision of the heel spur. A report on 38 cases. Acta Orthop Belg 2003; 69:267.
Trojian. T, Tucker. A, Plantar Fasciitis, Am Fam Physician. 2019 Jun 15;99(12):744-750.
Thompson J, Saini S, Reb C, Daniel J. Diagnosis and Management of Plantar Fasciitis: . Journal of Osteopathic Medicine. 2014;114(12): 900-901. https://doi.org/10.7556/jaoa.2014.177
Lim, A. T., How, C. H., & Tan, B. (2016). Management of plantar fasciitis in the outpatient setting. Singapore medical journal, 57(4), 168–171. https://doi.org/10.11622/smedj.2016069